Balloon kyphoplasty
Treating spine fractures can save lives
A study of over 850,000 Medicare VCF patients predicted that median life expectancy was 2.2 to 7.3 years greater for operated than non-operated patients.1
Benefits of balloon kyphoplasty
A study of over 2,000,000 Medicare VCF patients showed that only 15 patients need to be treated with kyphoplasty in order to save a life at one year compared to nonsurgical management.3
Early diagnoses make all the difference
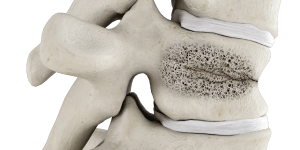
Acute and chronic pain in the elderly is commonly attributed to VCFs, often leading to further health deterioration in a “downward spiral” and a loss of independence. Because there is a substantial risk of subsequent fractures, it’s important that VCFs are diagnosed and treated early.
Procedure
1
Guide needle into fractured vertebra using fluoroscopy.
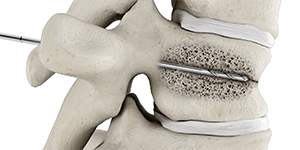
2
Insert hand drill into the anterior third of the vertebral body to create a pathway.
3
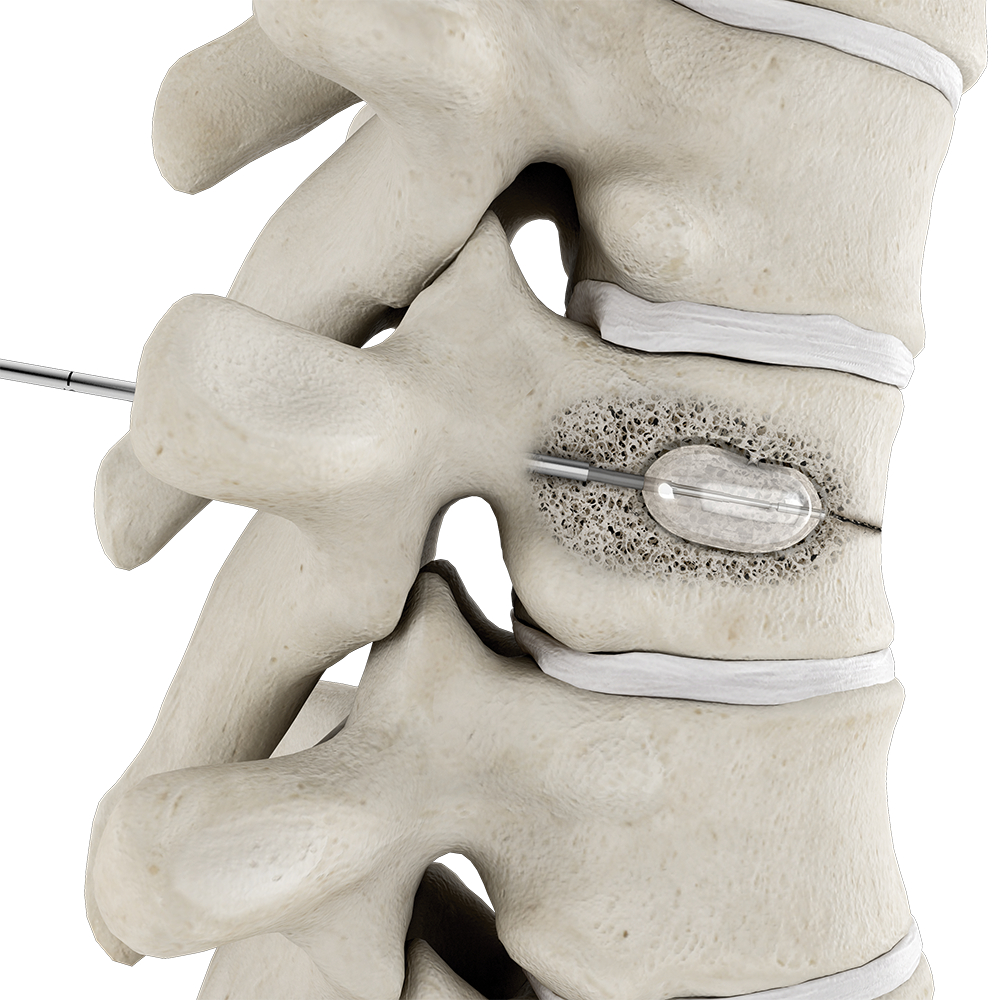
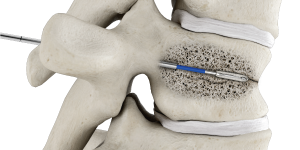
Insert balloon catheter into the fractured vertebra.
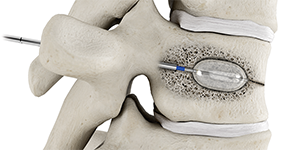
4
Inflate balloon, compacting the trabeculae and creating a cavity.
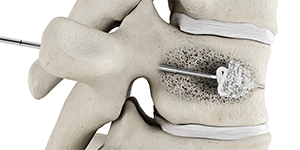
5
Once the balloon is deflated and withdrawn, fill the cavity with bone cement.
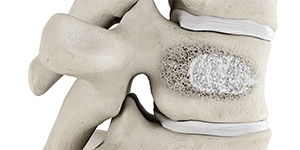
6
Stabilized vertebral body.

