
Vertebroplasty
Relief. Supported by over a decade of clinical evidence.
Vertebroplasty is a well-established treatment of vertebral compression fractures (VCFs). Over a decade of clinical studies have demonstrated positive outcomes following vertebroplasty for the treatment of VCFs.12345
The benefits of a vertebroplasty procedure:
Stabilize and strengthen
Vertebroplasty uses a specially formulated acrylic bone cement to stabilize and strengthen the fracture and surrounding vertebral body. It’s done on an outpatient basis and requires only a local anesthetic and mild sedation, eliminating the complications that may result from open surgery and general anesthesia.
Minimally invasive
Vertebroplasty is done through a small puncture in the skin (as opposed to an open incision).
Quick and simple
The procedure typically takes about 30 minutes to complete.
The clinical outcomes couldn’t be more clear
Studies have shown vertebroplasty to be a safe and effective treatment option for vertebral compression fractures.

Safe, effective and at an acceptable cost
The Vertos II study conducted by Klazen et al., P Lohle, J de Vries, et al.12 found vertebroplasty to be safe, effective, and at an acceptable cost for patients with acute osteoporotic VCFs. Additionally, the study concluded that vertebroplasty gives greater pain relief than conservative treatments.
90%
of patients experienced pain relief and improved mobility
A study by Jensen et al., AJ Evans, JM Mathis, DF Kallmes, HJ Cloft, and JE Dion13 showed that 90% of patients (29 patients with 47 fractures), suffering from age-related or steroid-induced osteoporosis, experienced pain relief and improved mobility at 24 hours post-procedure.
down arrow
Significant pain reduction
97%
patients had complete or partial pain relief15
A third study by Cotton et al., F Dewatre, B Cortet, R Assaker, D Leblond, and B Duquesnoy described complete or partial pain relief in 97% of patients who were treated for painful metastasis (29 patients) and multiple myeloma (8 patients).15
90%
success rate in the treatment of osteoporotic vertebral fractures
Results of a study on percutaneous vertebroplasty in 231 patients showed a 90% success rate in the treatment of osteoporotic vertebral fractures and an 80% success rate in painful or unstable neoplastic lesions and vertebral hemangiomas.16
The RDQ dropped to an average score of
11
A Mayo Clinic study concluded that patients (113 patients were treated at 164 vertebral levels) who underwent vertebroplasty experienced relief of back pain and symptoms, as shown by improvement in verbal pain and RDQ (Roland-Morris Disability Questionnaire) scores. The RDQ correlates well with measures of pain, shows clinically significant improvement, and is responsive to changes across time. Prior to treatment, the average RDQ score was 18 on a scale of 23. The RDQ dropped to an average score of 11 immediately after treatment and remained at that level throughout the year-long study.17
Procedure18
1
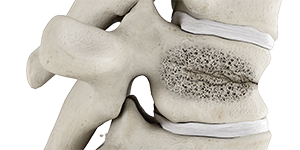
Vertebral compression fracture is identified

2
Needle is guided into fractured vertebra using fluoroscopy

3
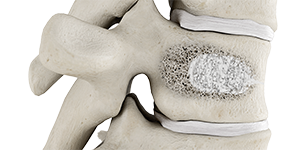
Bone cement is injected
4
Stabilized vertebral body

