
Sacroplasty
Improve your mobility. And your quality of life.1
Sacral insufficiency fractures (SIFs) are an often underdiagnosed condition in the elderly population, typically presenting with severe low back pain and resulting in immobility.
Risk factors for SIFs include:23
- Osteoporosis (most common)
- Radiation therapy
- Neoplasm
- Corticosteroid treatment
- Other comorbidities
50% of women and 25% of men will have an osteoporotic fracture in their lifetime4
Why choose sacroplasty?
A 2019 analysis suggests that sacroplasty is safe and effective for the treatment of osteoporotic or malignant sacral fractures. Statistically significant improvements in pain scores have been observed up to 12 months.5 Benefits can include the following:
Different SIF types
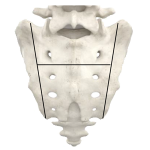
H-shaped fracture
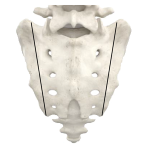
Bilateral vertical sacral fracture
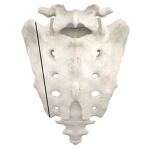
Unilateral vertical sacral fracture
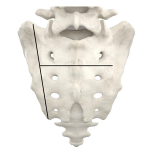
Combined unilateral vertical and horizontal fractures
What to expect with sacroplasty
View the step-by-step procedure

Before the procedure
Using x-ray guidance, one or more needles will be inserted into the sacrum through a small incision.
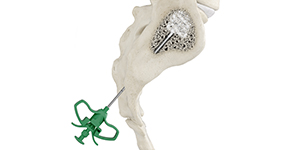
During the procedure
The sacrum is filled with bone cement to stabilize the fracture. As it hardens, the cement forms an internal cast that holds the sacrum in place. The incision will be covered with a bandage.

After the procedure
You will lie on your back for a short period of time while the cement continues to harden. Vital signs are monitored. Typically, you can go home within a few hours of treatment. If you notice any signs of wound infection, bleeding or hematoma, you should contact your healthcare provider immediately.

